Projected epidemiological trends and burden of liver cancer by 2040 based on GBD, CI5plus, and WHO data

Liver cancer incidence and mortality rates estimates in 2020 and comparison by HDI
According to the GLOBOCAN estimates, there were 905,000 new liver cancer incidence cases whereas 830,000 deaths worldwide in 2020. Globally, the crude rate and ASIR for liver cancer stood at 11.6 and 5.2 per 100,000 population, respectively. ASIRs of liver cancer pertinent to the males varied to 60-fold, with a range of ASIRs from 106.0 (Mongolia) to 1.6 (Botswana) for the different nations. High-income countries acknowledged a substantial burden of liver cancer, with the highest incidence rates observed in Eastern Asia (ASIR: 54.3 per 100,000 individuals), with Mongolia having the highest ASIR 85.6 per 100,000 individuals (Table 1).
On a global scale in 2020, crude rate and ASMR were 10.7 and 4.8 per 100,000 individuals, respectively. The highest mortality rate (ASR, 80.6 per 100,000 individuals) was observed in Mongolia, whereas the lowest mortality rate (ASR, 1.1 per 100,000 individuals) was observed in Sri Lanka (Fig. 1). In various continents or regions, higher mortality rates were observed in Northern Africa (ASR, 10 per 100,000 individuals), Melanesia (ASR, 8.9 per 100,000 individuals), and Eastern Asia (ASR, 8 per 100,000 individuals) (Table 1).

Liver cancer-related incidence and mortality rates estimates in 2020 for different age groups among males or females. (A) Age-standardized incidence rates (ASIR) and (B) Age-standardized mortality rates (ASMR).
Table 1 described estimated liver cancer burden by HDI status. Countries with a high HDI contributed to 60.6% of liver cancer cases and 63.2% of liver cancer related deaths. In contrast, medium and low HDI countries were responsible for only 14.7% of liver cancer cases but accounted for 15.4% of liver cancer deaths (Table 1). In our study, we observed a more than two-fold increase in ASIRs in high HDI countries compared to populations in countries with a very high HDI. Additionally, ASMRs were nearly three times higher. The correlation analysis using Pearson’s method illustrates the association between case fatality rates of liver cancer and HDI levels, as shown in Fig. S1. Across all 185 countries, there was an observed decrease in the case fatality rates of liver cancer with higher HDI levels (R = − 0.59, P < 2.2e−16). The case fatality rates for high HDI, moderate HDI, and low HDI are comparable, each around 95%, while the case fatality rate for very high HDI is comparatively lower (Table 1). Notably, the ASIRs for liver cancer were consistently high, exceeding 70%, across all HDI levels, ranging from 72.86 to 96.77%.
In terms of global regions, only Australia and New Zealand, as well as North America, exhibited liver cancer case fatality rates below 70%. In contrast, Africa, Asia, Latin America, and the Caribbean all recorded rates exceeding 90%. Especially, Melanesia was reported with the highest reported case fatality rate for liver cancer reaching an extraordinary 100%. The ASRs for liver cancer incidence and mortality were consistently higher among males when compared to females across all continents and regions, indicating substantial gender disparities.
The Male: Female ratios for incidence ranged from 1.8 in low HDI countries to 2.8 in high HDI and very high HDI countries. Similarly, the mortality Male: Female ratios followed the same range. The incidence and mortality of Micronesia has the largest difference between men and women, the ASIR of Male: Female ratio is 4.6, and the ASMR of Male: Female ratio is 3.6 (Table 1). No correlation was observed between a country’s HDI and ASRs for liver cancer incidence or mortality when considering gender differences (Fig. S2).
HIV prevalence and liver cancer
HIV could potentially contribute to the development of specific types of liver cancer.
However, the connection with this broader category of liver cancer remained uncertain. The correlation between HIV prevalence in 2020 and the estimated ASIR of liver cancer for both sexes combined was given (Fig. 2). These estimates of HIV prevalence varied depending on country and region, but a correlation between a HIV incidence in a country and ASRs for liver cancer incidence was not observed.

Significantly, a nonlinear correlation was observed between HBsAg and ASIRs. The ASIR of liver cancer exhibited a notable increasing trend with the increase in HBsAg prevalence until it reached 13.
Our study employed a generalized additive model to investigate the correlation between ASIRs of liver cancer and various factors such as HIV and HBsAg. Notably, a nonlinear relationship was observed between HBsAg and ASIRs. Before the prevalence of HBsAg reached 13, the ASIR of liver cancer demonstrated a significant increase with the rise of HBsAg (p < 0.001) (Fig. 2). While the direct relationship between HIV and ASIR was not directly observed, the establishment of a generalized additive model involving HBsAg and HIV revealed an upward trend in HBsAg as HIV increased before the HIV prevalence reached 1 (p < 0.001) (Fig. 3). Applying the same model to explore the connection between the incidence and mortality of liver cancer and lifestyle risk factors by genders, we found that obesity and insufficient physical activity had a reverse impact on the ASIR and ASMR of liver cancer. Additionally, there was a positive linear relationship between obesity and insufficient physical activity. Smoking exhibited differential effects on liver cancer incidence and mortality in men and women (Figs. S3–S6).

While a direct relationship between HIV and ASIR was not directly observed, the creation of a generalized additive model (GAM) incorporating HBsAg and HIV described an increasing trend in HBsAg as HIV prevalence increased, up to the point where HIV prevalence reached 1.
Global incidence trends of liver cancer and HDI
Liver cancer in the elderly imposes a considerable disease burden, with the highest incidence occurring at the age of 60 or older, making a significant contribution to the overall incidence. The study observed relatively stable truncated ASIRs36 of liver cancer in 25 out of 45 countries, while they exhibited significant fluctuations in 10 countries, notably Uganda. In the United States, truncated ASIRs among individuals younger than 60 years old were increasing, while those among individuals older than 60 years old were decreasing (Fig. S7). In the male population, incidence increased in 32 countries, with AAPCs ranging from 0.3 to 7.7, as illustrated in Fig. 4A. Out of the 32 countries with increasing trends, especially in Northern Europe, Iceland (AAPC, 7.7 [95% CI 3.9–11.6]) and Ireland (AAPC, 6.1 [95% CI 4.3–8.0]) reported with a higher rate of incidence. In contrast, among countries with decreasing trends, the AAPCs for liver cancer incidence were decreased in Southern Europe, South America, and Asia. Particularly, Japan (AAPC, − 3.5 [95% CI − 3.9 to − 3.0]), Chile (AAPC, − 2.1 [95%CI − 7.2 to − 3.6]), and China (AAPC, − 2.4 [95% CI − 2.9 to − 1.9]) exhibited a downward trend of higher than 2%.
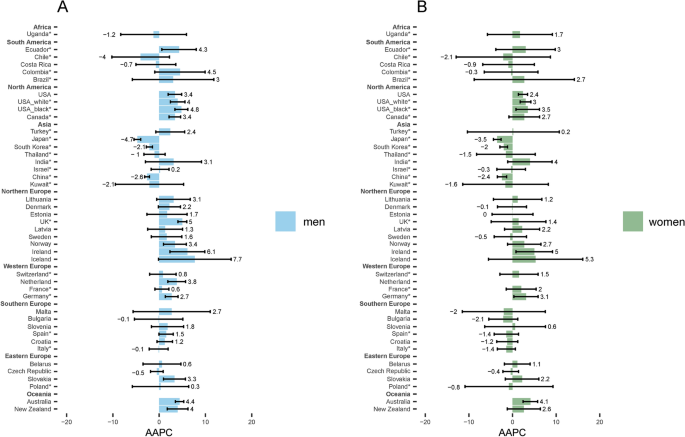
(A) Among the male population, liver cancer incidence surged in 32 countries, with Average Annual Percent Changes (AAPCs) spanning from 0.3 to 7.7. (B) In the case of women in Iceland, Ireland, and Australia, the age-standardized incidence rates (ASIRs) demonstrated annual increases of 5.3%, 5.0%, and 4.1%, respectively. In gender-specific subgroups, more countries exhibited a downward trend for women than for men.
In case of women (Fig. 4B), in Iceland, Ireland and Australia, the ASIRs have enhanced by 5.3%, 5.0%, and 4.1%, respectively on annual basis. Among the 41 countries, these three nations observed the most substantial growth rates. In gender-specific subgroups, there were more countries exhibiting a declining trend for women than for men.
Liver cancer incidence rates have increased among the nations with high ASIRs; a notable increase was observed in the nations with the lowest ASIRs, mainly among the individuals aged older than 60 years (Fig. 5). The association between ASIR and the HDI was not clearly delineated, as similar ASIRs were observed in both low and high HDI countries. However, as the ASIR increased in 1998, highly developed nations exhibited a convergence around an AAPC of 2.5% for individuals under the age of 60. This indicates that despite variations in HDI, the trend in ASIR among developed countries showed a consistent increase in younger populations.

(A, B) Liver cancer incidence rates have risen in nations with high age-standardized incidence rates (ASIRs), and a significant increase has been observed in nations with the lowest ASIRs, particularly among individuals aged over 60 years.
The incidence of liver cancer showed an increase in 38 populations (AAPCs, 0.1–6.2) among individuals under the age of 60. Substantial rise in the morbidity rates were observed in Thailand (AAPC, 6.2 [95% CI 4.5–7.8]), Slovenia (AAPC, 4.5 [95% CI 2.8–6.2]), and South Korea (AAPC, 4.4 [95% CI 4.0–6.9]). A similar trend was observed for the individuals older than 60, as ASIRs increased in 24 countries (AAPCs, 0.2–6.6). Furthermore, a notable increase was observed in Bahrain (AAPC, 6.6 [95% CI 2.6–10.8]), Ecuador (AAPC, 5.4 [95% CI 2.3–8.5]), and Thailand (AAPC, 4.2 [95% CI 2.3–6.1]) (Fig. 5).
In individuals under 75 years of age, significant increases in liver cancer incidence were observed in 30 populations. The most pronounced rises were recorded in Thailand (AAPC: 5.6 [95% CI 4.4–6.9]), Turkey (AAPC: 5.3 [95% CI 2.9–7.8]), and South Korea (AAPC: 4.3 [95% CI 3.2–5.5]) (Fig. S9). Additionally, approximately one-third of the countries showed increasing ASIRs over a 15-year period in the subgroup of patients aged 75 years or older (Fig. S9).
Global mortality trends of liver cancer
In various age groups, mortality rates have generally been decreasing across most continents and regions, with the exception of northern Europe and western Europe, where rates have increased in the recent years. The United Kingdom and Canada were reported to be with the higher mortality rates in Europe and America, respectively. The ASMRs for liver cancer exhibited a significant downward trend (AAPC, − 10.9 [95% CI − 17.0 to − 4.3]) among the individuals aged 60 and older in Bahrain. While there was an overall increase in rates for female patients in several regions, over half of the countries reported a decreasing AAPC of ASMRs, with decline ranging from 0.2 to 4.5% (Fig. 6).

(A, B) The age-standardized mortality rates (ASMRs) for liver cancer showed a significant decline (AAPC, − 10.9 [95% CI − 17.0 to − 4.3]) among the individuals aged 60 and older in Bahrain. Although there was a general increase in rates for female patients in various regions, more than half of the countries reported a decreasing AAPC of ASMRs, with decline ranging from 0.2 to 4.5%.
The AAPC of ASMRs increased for individuals under 75 years of age and decreased for those aged 75 years and older for certain countries such as Chile, Turkey, and Sweden (Fig. S8). In conclusion, the percentage change in the ASMR differed significantly among the nations, but the disparities between age groups are not as obvious as those between gender groups (Fig. S10).
Global trends of age-standardized DALY rates, the percent of DALYs of liver cancer and burden attributable to smoking, alcohol use and high BMI
In 2019, liver cancer contributed to a global age-standardized DALYs rate of 161.92, accompanied by the 23% reduction when compared to the rate recorded in 1990. During this period, age-standardized DALYs have increased in many regions, include North America, Western Europe, North Africa and Middle East nations. Age-standardized DALYs have stabilized in specific regions, including South Asia, Latin America, and the Caribbean. The incidence of liver cancer increased annually until 1996 subsequently decreased annually; thereafter, a significant decline in age-standardized DALY rates were remarkably decreased by 46% between 1996 and 2019. In 2019, approximately 46.3% of liver cancer-related DALYs in both sexes were linked to hepatitis B globally, whereas 23% to hepatitis C, 17.4% to alcohol use, 6.4% to non-alcoholic steatohepatitis (NASH), and 7% to other causes. Among men, liver cancer DALYs in most regions were primarily attributable to hepatitis B and alcohol use, while almost were attributed to C for women except for Sub-Saharan Africa, Southeast Asia, East Asia, and Oceania, which were attributed to hepatitis B. High-income Asia Pacific was associated with a higher liver cancer DALYs which reached to 491.4% (Figs. 7A–B and 8A).

(A, B) Among men, liver cancer Disability-Adjusted Life Years (DALYs) in most regions were primarily linked to hepatitis B and alcohol use, while almost all were attributed to hepatitis C for women, except for Sub-Saharan Africa, Southeast Asia, East Asia, and Oceania, where hepatitis B played a significant role. High-income Asia Pacific showed a higher prevalence of liver cancer DALYs, reaching 491.4%. Globally, smoking, alcohol use, and high body-mass index were major contributors to age-standardized DALYs, constituting proportions of 16.96%, 19%, and 12.88%, respectively. These contributions were generally higher in males compared to females, particularly for smoking and alcohol use.

(A, B) Estimated number of new liver cancer cases and deaths from 2020 to 2040. Predicted number of new liver cancer cases and deaths by HDI classification, assuming seven scenarios of annual change in global rates between 2020 and 2040, for both sexes and all age groups (0–85+). Countries or regions with low HDI are projected to experience a significant increase of 101% in both incidence and mortality pertinent to liver cancer from 2020 to 2040, highlighting their increased vulnerability. Conversely, high HDI countries are expected to see a substantial increase of 150.2% in both incidence and mortality among individuals aged 75 years and older by 2040, based on GLOBOCAN global rates estimated in 2020.
On a global scale, smoking, alcohol use, and high body-mass index were significant contributors to age-standardized DALYs, accounting for proportions of 16.96%, 19%, and 12.88%, respectively. These contributions were typically higher in males when compared to females, particularly for smoking and alcohol use (Fig. 8B). The highest proportion of age-standardized DALYs (24.02%) was evident in the high-income North America because of increased body-mass index. These findings align with previously identified risk factors linked to morbidity and mortality.
Future global liver cancer burden in 2040
Assuming that ASIR in 2020 remains unchanged, the anticipated global number of new liver cancer cases is expected to increase from around 905,347 to an estimated 1,392,474 by 2040, reflecting a corresponding growth of 53.8% over a span of 20 years. Nations or regions in transitional economies with low HDI exhibit heightened vulnerability, with a significant surge of 101% in both incidence and mortality from 2020 to 2040 (Fig. 9A–B). High HDI countries are expected to undergo a substantial rise of 150.2% in both incidence and mortality by 2040 among the individuals aged 75 years and older, based on global rates estimated in 2020 (Fig. 9C–D). In addition to the demographic shifts influencing the population base, we also considered the impact of risk factors on the changes in ASRs. Our predictions encompassed seven scenarios, each representing annual changes in ASRs ranging from − 3% to + 3%. In low HDI countries, all scenarios indicated a potential increase in the annual number of liver cancer cases and deaths by 2040. Notably, the difference between the predicted new cases and deaths of liver cancer by 2040 was minimal, particularly in low and medium HDI countries. This suggests a consistent rise in both incidence and mortality regardless of the specific scenario. These findings elucidate the significant burden of liver cancer expected in low and medium HDI countries, driven by both population growth and increased exposure to risk factors. The projected trends highlight the urgent need for targeted public health interventions and policies aimed at mitigating risk factors and improving cancer outcomes in these vulnerable regions (Fig. 10).

(A–D) In case of ASIR during 2020 remains unchanged, the future projections of liver cancer cancers is anticipated to enhanced in both sexes; mainly, the regions in transitional economies with minimal HDI resulted in a higher vulnerability, accompanied by the typical raise of 101% in both incidence as well as mortality from the period of 2020 to 2040. In case of nations with high HDI are expected to be associated with a greater enhancement in both incidence and morality by 2040 typically among the individuals of age greater than 75 years depending on global rates estimated in 2020.
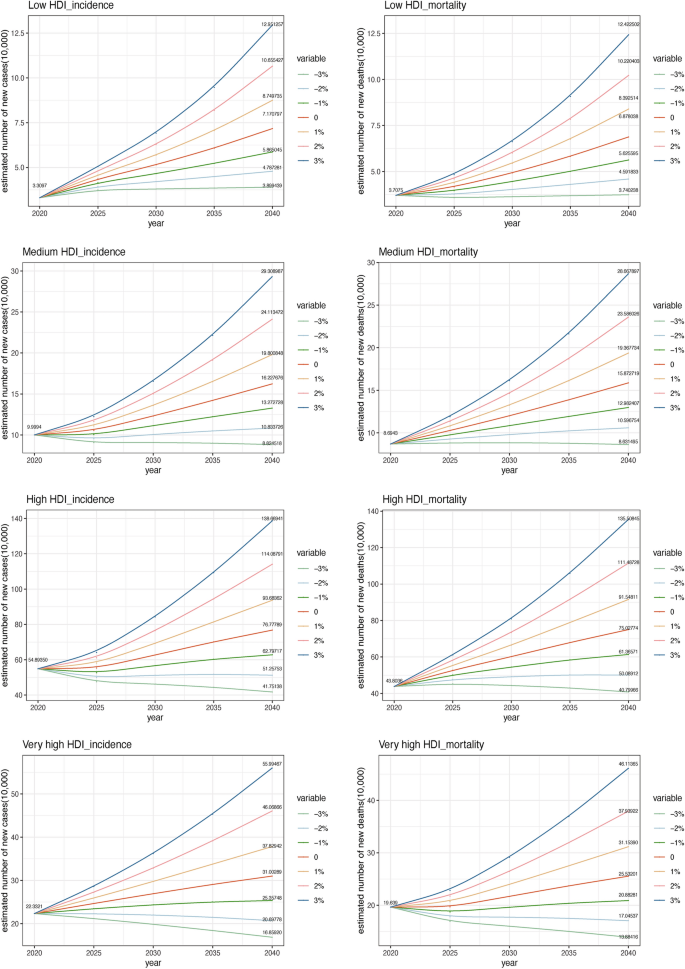
Projected trends of liver cancer incidence and mortality by 2040 depending on the low HDI, medium HDI, high HDI and very high HDI and the projection predictions are encompassed in the range of each representing annual changes in ASRs ranging from − 3% to + 3%.
link







