Health inequalities in hepatocellular carcinoma surveillance, diagnosis, treatment, and survival in the United Kingdom: a scoping review
Burton A, Tataru D, Driver RJ, Bird TG, Huws D, Wallace D, et al. Primary liver cancer in the UK: Incidence, incidence-based mortality, and survival by subtype, sex, and nation. JHEP Rep. 2021;3:100232. https://doi.org/10.1016/j.jhepr.2021.100232
Google Scholar
Smittenaar CR, Petersen KA, Stewart K, Moitt N. Cancer incidence and mortality projections in the UK until 2035. Br J Cancer. 2016;115:1147–55. https://doi.org/10.1038/bjc.2016.304
Google Scholar
Shelton J, Zotow E, Smith L, Johnson SA, Thomson CS, Ahmad A, et al. 25 year trends in cancer incidence and mortality among adults aged 35-69 years in the UK, 1993-2018: retrospective secondary analysis. BMJ. 2024;384:e076962 https://doi.org/10.1136/bmj-2023-076962
Google Scholar
Suddle A, Reeves H, Hubner R, Marshall A, Rowe I, Tiniakos D, et al. British Society of Gastroenterology guidelines for the management of hepatocellular carcinoma in adults. Gut. 2024;73:1235–68.
Google Scholar
NHS England. Hepatocellular carcinoma: delivering quality ultrasound surveillance 2024 [Available from: https://www.england.nhs.uk/long-read/hepatocellular-carcinoma-delivering-quality-ultrasound-surveillance/#guidance-statements.
Liver Cancer UK. Liver Cancer – A Call to action. British Liver Trust; 2023.
NHS England. Hepatocellular carcinoma surveillance: minimum standards 2024 [Available from: https://www.england.nhs.uk/long-read/hepatocellular-carcinoma-surveillance-minimum-standards/.
Jones PD, Lai JC, Bajaj JS, Kanwal F. Actionable Solutions to Achieve Health Equity in Chronic Liver Disease. Clin Gastroenterol Hepatol. 2023;21:1992–2000. https://doi.org/10.1016/j.cgh.2023.03.043
Google Scholar
Kondili LA, Lazarus JV, Jepsen P, Murray F, Schattenberg JM, Korenjak M, et al. Inequities in primary liver cancer in Europe: The state of play. J Hepatol. 2024;80:645–60. https://doi.org/10.1016/j.jhep.2023.12.031
Google Scholar
World Health Organization. Health inequalities and their causes 2018 [Available from: www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes.
Ventura-Cots M, Bataller R, Lazarus JV, Benach J, Pericàs JM. Applying an equity lens to liver health and research in Europe. J Hepatol. 2022;77:1699–710. https://doi.org/10.1016/j.jhep.2022.07.021
Google Scholar
Liao W, Coupland CAC, Innes H, Jepsen P, Matthews PC, Campbell C, et al. Disparities in care and outcomes for primary liver cancer in England during 2008-2018: a cohort study of 8.52 million primary care population using the QResearch database. eClinicalMed. 2023;59. https://doi.org/10.1016/j.eclinm.2023.101969.
Burton A, Balachandrakumar VK, Driver RJ, Tataru D, Paley L, Marshall A, et al. Regional variations in hepatocellular carcinoma incidence, routes to diagnosis, treatment and survival in England. Br J Cancer. 2022;126:804–14. https://doi.org/10.1038/s41416-021-01509-4
Google Scholar
Beecroft S, O’Connell M, Nassar A, Noon K, Pollock KG, Palmer D, et al. Major variation in hepatocellular carcinoma treatment and outcomes in England: A retrospective cohort study. Frontline Gastroenterol. 2022;14:19–24. https://doi.org/10.1136/flgastro-2022-102142
Google Scholar
Marmot M Fair Society, Healthy Lives. 2010
Alderwick H, Dixon J The NHS long term plan. British Medical Journal Publishing Group; 2019.
NHS England. Core20PLUS5 (adults) – an approach to reducing healthcare inequalities 2021 [Available from: https://www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement-programme/core20plus5/.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143 https://doi.org/10.1186/s12874-018-0611-x
Google Scholar
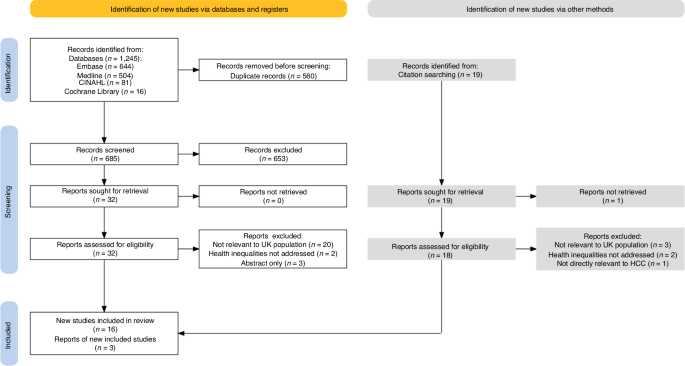
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Google Scholar
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Google Scholar
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14:579 https://doi.org/10.1186/s12913-014-0579-0
Google Scholar
Haddaway NR, Page MJ, Pritchard CC, McGuinness LA. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst Rev. 2022;18:e1230.
Google Scholar
Webb GJ, Hodson J, Chauhan A, O’Grady J, Neuberger JM, Hirschfield GM, et al. Proximity to transplant center and outcome among liver transplant patients. Am J Transpl. 2019;19:208–20. https://doi.org/10.1111/ajt.15004
Google Scholar
Farrell C, Halpen A, Cross TJ, Richardson PD, Johnson P, Joekes EC. Ultrasound surveillance for hepatocellular carcinoma: service evaluation of a radiology-led recall system in a tertiary-referral centre for liver diseases in the UK. Clin Radio. 2017;72:338.e11–.e17. https://doi.org/10.1016/j.crad.2016.10.019
Google Scholar
Hamill V, Gelson W, MacDonald D, Richardson P, Ryder SD, Aldersley M, et al. Delivery of biannual ultrasound surveillance for individuals with cirrhosis and cured hepatitis C in the UK. Liver Int. 2023;43:917–27. https://doi.org/10.1111/liv.15528
Google Scholar
Dharmarajan KV, Presley CJ, Wyld L. Care Disparities Across the Health Care Continuum for Older Adults: Lessons From Multidisciplinary Perspectives. Am Soc Clin Oncol Educ Book. 2021;41:e215–e24. https://doi.org/10.1200/edbk_319841
Google Scholar
Konfortion J, Coupland VH, Kocher HM, Allum W, Grocock MJ, Jack RH. Time and deprivation trends in incidence of primary liver cancer subtypes in England. J Evaluation Clin Pr. 2014;20:498–504. https://doi.org/10.1111/jep.12188
Google Scholar
Ladep NG, Khan SA, Crossey MM, Thillainayagam AV, Taylor-Robinson SD, Toledano MB. Incidence and mortality of primary liver cancer in England and Wales: changing patterns and ethnic variations. World J Gastroenterol. 2014;20:1544–53. https://doi.org/10.3748/wjg.v20.i6.1544
Google Scholar
Jack RH, Konfortion J, Coupland VH, Kocher HM, Berry DP, Allum W, et al. Primary liver cancer incidence and survival in ethnic groups in England, 2001–2007. Cancer Epidemiol. 2013;37:34–8. https://doi.org/10.1016/j.canep.2012.10.008
Google Scholar
West J, Wood H, Logan RF, Quinn M, Aithal GP. Trends in the incidence of primary liver and biliary tract cancers in England and Wales 1971-2001. Br J Cancer. 2006;94:1751–8. https://doi.org/10.1038/sj.bjc.6603127
Google Scholar
Haworth EA, Soni Raleigh V, Balarajan R. Cirrhosis and Primary Liver Cancer Amongst First Generation Migrants in England and Wales. Ethnicity Health. 1999;4:93–9. https://doi.org/10.1080/13557859998227
Google Scholar
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660
Google Scholar
Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. Hepatocellular carcinoma. Nat Rev Dis Prim. 2021;7:6 https://doi.org/10.1038/s41572-020-00240-3
Google Scholar
Rigamonti C, Andorno S, Maduli E, Capelli F, Boldorini R, Sartori M. Gender and liver fibrosis in chronic hepatitis: the role of iron status. Alimentary Pharm therapeutics. 2005;21:1445–51.
Google Scholar
Chavda V, Zajac KK, Gunn JL, Balar P, Khadela A, Vaghela D, et al. Ethnic differences in hepatocellular carcinoma prevalence and therapeutic outcomes. Cancer Reports. 2023;6 (no pagination) https://doi.org/10.1002/cnr2.1821.
Yip TCF, Vilar‐Gomez E, Petta S, Yilmaz Y, Wong GLH, Adams LA, et al. Geographical similarity and differences in the burden and genetic predisposition of NAFLD. Hepatology. 2023;77:1404–27. https://doi.org/10.1002/hep.32774
Google Scholar
Ministry of Housing Communities & Local Government. People living in deprived neighbourhoods 2020 [Available from: https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/demographics/people-living-in-deprived-neighbourhoods/latest/#data-sources.
Okolie C, Hookway A, Wale A, Everitt J, Shaw H, Lewis R, et al. A rapid review of barriers and facilitators to cancer screening uptake (breast, cervical and bowel) in underserved populations. medRxiv. 2022:2022.08.11.22278362 https://doi.org/10.1101/2022.08.11.22278362.
Marmot M. Health equity in England: the Marmot review 10 years on. BMJ. 2020:m693 https://doi.org/10.1136/bmj.m693.
Rashid T, Bennett JE, Muller DC, Cross AJ, Pearson-Stuttard J, Asaria P, et al. Mortality from leading cancers in districts of England from 2002 to 2019: a population-based, spatiotemporal study. Lancet Oncol. 2024;25:86–98. https://doi.org/10.1016/S1470-2045(23)00530-2
Google Scholar
Curran C, Stanley AJ, Barclay ST, Priest M, Graham J. The association between deprivation and the incidence and survival of patients with hepatocellular carcinoma in the West of Scotland. Expert Rev Gastroenterol Hepatol. 2021;15:1427–33. https://doi.org/10.1080/17474124.2021.1997586
Google Scholar
Parkin DM, Boyd L, Walker LC. 16. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer. 2011;105:S77–81. https://doi.org/10.1038/bjc.2011.489
Google Scholar
Williams R, Aspinall R, Bellis M, Camps-Walsh G, Cramp M, Dhawan A, et al. Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatitis. Lancet. 2014;384:1953–97. https://doi.org/10.1016/S0140-6736(14)61838-9
Google Scholar
Haq MI, Drake TM, Goh TL, Ahmed A, Forrest E, Barclay S, et al. Effect of Hepatocellular Carcinoma Surveillance Programmes on Overall Survival in a Mixed Cirrhotic UK Population: A Prospective, Longitudinal Cohort Study. J Clin Med. 2021;10:2770.
Google Scholar
Tan DJH, Ng CH, Lin SY, Pan XH, Tay P, Lim WH, et al. Clinical characteristics, surveillance, treatment allocation, and outcomes of non-alcoholic fatty liver disease-related hepatocellular carcinoma: a systematic review and meta-analysis. Lancet Oncol. 2022;23:521–30. https://doi.org/10.1016/s1470-2045(22)00078-x
Google Scholar
Hydes TJ, Cuthbertson DJ, Palmer DH, Elshaarawy O, Johnson PJ, Fernando R, et al. Ultrasonography in surveillance for hepatocellular carcinoma in patients with non-alcoholic fatty liver disease. Hepatoma Res. 2023;9:12. https://doi.org/10.20517/2394-5079.2022.97
Google Scholar
Selvapatt N, House H, Brown A. Hepatocellular Carcinoma Surveillance: Are We Utilizing It? J Clin Gastroenterol. 2016;50:e8–e12. https://doi.org/10.1097/MCG.0000000000000344
Google Scholar
Singal AG, Pillai A, Tiro J. Early Detection, Curative Treatment, and Survival Rates for Hepatocellular Carcinoma Surveillance in Patients with Cirrhosis: A Meta-analysis. PLOS Med. 2014;11:e1001624. https://doi.org/10.1371/journal.pmed.1001624
Google Scholar
van Meer S, de Man RA, Coenraad MJ, Sprengers D, van Nieuwkerk KM, Klümpen HJ, et al. Surveillance for hepatocellular carcinoma is associated with increased survival: Results from a large cohort in the Netherlands. J Hepatol. 2015;63:1156–63. https://doi.org/10.1016/j.jhep.2015.06.012
Google Scholar
Scott RA, Cross TJS, Clarke C, Khan SA, Ryder SD, Franklin J, et al. Outcomes of National Survey of the Practice of Hepatocellular Carcinoma Surveillance. J Hepatocell Carcinoma. 2023;10:725–31. https://doi.org/10.2147/jhc.s403702
Google Scholar
Cross TJS, Villanueva A, Shetty S, Wilkes E, Collins P, Adair A, et al. A national survey of the provision of ultrasound surveillance for the detection of hepatocellular carcinoma. Frontline Gastroenterol. 2016;7:82–9. https://doi.org/10.1136/flgastro-2015-100617
Google Scholar
Ramai D, Singh J, Chandan S, Tartaglia N, Ambrosi A, Khan SR, et al. Utilization of Hepatocellular Carcinoma Surveillance Programs in Patients with Cirrhosis: A Systematic Review and Meta-Analysis. J Clin Gastroenterol. 2023;57:198–203. https://doi.org/10.1097/MCG.0000000000001668
Google Scholar
Wolf E, Rich NE, Marrero JA, Parikh ND, Singal AG. Use of Hepatocellular Carcinoma Surveillance in Patients With Cirrhosis: A Systematic Review and Meta‐Analysis. Hepatology. 2021;73:713–25. https://doi.org/10.1002/hep.31309
Google Scholar
Zhao, Jin M, Le RH, Le MH, Chen VL, Jin M, et al. Poor adherence to hepatocellular carcinoma surveillance: A systematic review and meta-analysis of a complex issue. Liver Int. 2018;38:503–14. https://doi.org/10.1111/liv.13555
Google Scholar
Ladhani S, Ohri A, Wong RJ. Disparities in Hepatocellular Carcinoma Surveillance: Dissecting the Roles of Patient, Provider, and Health System Factors. J Clin Gastroenterol. 2020;54:218–26. https://doi.org/10.1097/MCG.0000000000001313
Google Scholar
Singal AG, Tiro JA, Murphy CC, Blackwell JM, Kramer JR, Khan A, et al. Patient-Reported Barriers Are Associated With Receipt of Hepatocellular Carcinoma Surveillance in a Multicenter Cohort of Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2021;19:987–95. https://doi.org/10.1016/j.cgh.2020.06.049.
Google Scholar
Goldberg DS, Taddei TH, Serper M, Mehta R, Dieperink E, Aytaman A, et al. Identifying barriers to hepatocellular carcinoma surveillance in a national sample of patients with cirrhosis. Hepatology. 2017;65:864–74. https://doi.org/10.1002/hep.28765
Google Scholar
Shaw J, Patidar KR, Reuter B, Hajezifar N, Dharel N, Wade JB, et al. Focused Education Increases Hepatocellular Cancer Screening in Patients with Cirrhosis Regardless of Functional Health Literacy. Digestive Dis Sci. 2021;66:2603–9. https://doi.org/10.1007/s10620-020-06583-x
Google Scholar
Geh D, Watson R, Sen G, French JJ, Hammond J, Turner P, et al. COVID-19 and liver cancer: lost patients and larger tumours. BMJ Open Gastroenterol. 2022;9:e000794. https://doi.org/10.1136/bmjgast-2021-000794
Google Scholar
American College of Radiology. LI-RADS® US Surveillance v2024 Core2024. Available from: https://www.acr.org/-/media/ACR/Files/RADS/LI-RADS/LI-RADS-US-Surveillance-v2024-Core.pdf.
American College of Radiology. CT/MRI LI-RADS® v2018 CORE2018. Available from: https://www.acr.org/-/media/ACR/Files/RADS/LI-RADS/LI-RADS-2018-Core.pdf.
Llovet JM, Zucman-Rossi J, Pikarsky E, Sangro B, Schwartz M, Sherman M, et al. Hepatocellular carcinoma. Nat Rev Dis Prim. 2016;2:16018. https://doi.org/10.1038/nrdp.2016.18
Google Scholar
Ambroggi M, Biasini C, Giovane CD, Fornari F, Cavanna L. Distance as a barrier to cancer diagnosis and treatment: Review of the literature. Oncologist. 2015;20:1378–85. https://doi.org/10.1634/theoncologist.2015-0110
Google Scholar
Fleurbaey M, Schokkaert E. Unfair inequalities in health and health care. J Health Econ. 2009;28:73–90. https://doi.org/10.1016/j.jhealeco.2008.07.016
Google Scholar
Kudo M. Management of Hepatocellular Carcinoma in Japan as a World-Leading Model. Liver Cancer. 2018;7:134–47. https://doi.org/10.1159/000484619
Google Scholar
Erreygers G, Van Ourti T. Measuring socioeconomic inequality in health, health care and health financing by means of rank-dependent indices: a recipe for good practice. J Health Econ. 2011;30:685–94. https://doi.org/10.1016/j.jhealeco.2011.04.004
Google Scholar
European Association for the Study of the Liver. Policy Statement Risk-based surveillance for hepatocellular carcinoma among patients with cirrhosis 2023 [Available from: https://easl.eu/wp-content/uploads/2023/04/Policy-Statement-Liver-Cancer-Screening_VFF.pdf.
Chan H, Vogel A, Berg T, De Toni E, Kudo M, Trojan J, et al. A comparative analysis of Elecsys GALAD and Elecsys GAAD score to detect early-stage hepatocellular carcinoma in an international cohort. J Hepatol. 2022;77:S937. https://doi.org/10.1016/S0168-8278(22)02154-7
Google Scholar
Tayob N, Kanwal F, Alsarraj A, Hernaez R, El-Serag HB. The Performance of AFP, AFP-3, DCP as Biomarkers for Detection of Hepatocellular Carcinoma (HCC): A Phase 3 Biomarker Study in the United States. Clin Gastroenterol Hepatol. 2023;21:415–23. https://doi.org/10.1016/j.cgh.2022.01.047.
Google Scholar
Singal AG, Tayob N, Mehta A, Marrero JA, El‐Serag H, Jin Q, et al. GALAD demonstrates high sensitivity for HCC surveillance in a cohort of patients with cirrhosis. Hepatology. 2022;75:541–9. https://doi.org/10.1002/hep.32185
Google Scholar
Fan R, Papatheodoridis G, Sun J, Innes H, Toyoda H, Xie Q, et al. aMAP risk score predicts hepatocellular carcinoma development in patients with chronic hepatitis. J Hepatol. 2020;73:1368–78. https://doi.org/10.1016/j.jhep.2020.07.025
Google Scholar
El-Serag H, Kanwal F, Ning J, Powell H, Khaderi S, Singal AG, et al. Serum biomarker signature is predictive of the risk of hepatocellular cancer in patients with cirrhosis. Gut. 2024. https://doi.org/10.1136/gutjnl-2024-332034.
Kanwal F, Khaderi S, Singal AG, Marrero JA, Asrani SK, Amos CI, et al. Risk Stratification Model for Hepatocellular Cancer in Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2023;21:3296–304.e3. https://doi.org/10.1016/j.cgh.2023.04.019.
Innes H, Nahon P. Statistical perspectives on using hepatocellular carcinoma risk models to inform surveillance decisions. J Hepatol. 2023;79:1332–7. https://doi.org/10.1016/j.jhep.2023.05.005
Google Scholar
link